Erika Krumbeck, ND, FABNP
Read time: 3 minutes
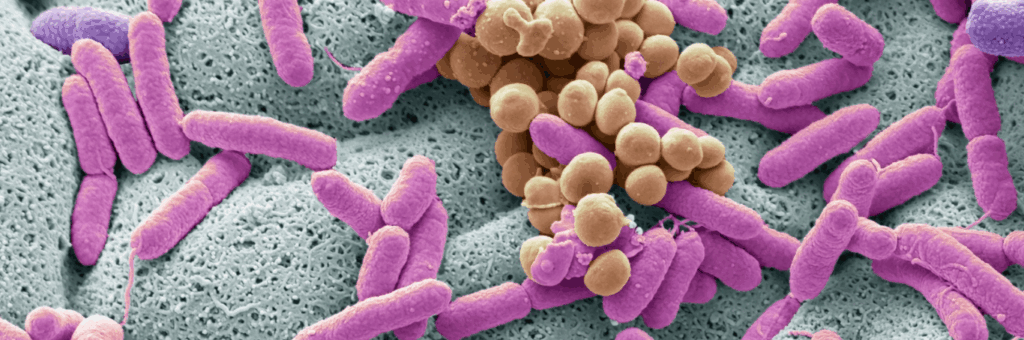
Childhood obesity is a complex condition shaped by far more than calorie intake. Inflammation, metabolic signaling, and the gut microbiome all play a role—and targeting the gut ecosystem has become a growing area of research. A new systematic review explores whether microbiome-based therapies can shift outcomes for pediatric obesity. Here’s what the evidence tells us—and what it doesn’t.
Grounding the Question: Can the Microbiome Help Address Pediatric Obesity?
There’s no doubt the gut microbiome is integral to metabolic health. In children and adolescents, obesity is frequently associated with gut dysbiosis—lower microbial diversity, reduced short-chain fatty acid (SCFA) production, and an overgrowth of pro-inflammatory taxa. Since the microbiome continues to mature into early adulthood, interventions during childhood may hold potential for long-term impact.
That said, when we look at the data, the outcomes are modest at best.
What the Review Found
A 2025 systematic review analyzed 17 randomized controlled trials (838 participants), testing five types of microbiome-directed therapies:
- Fecal Microbiota Transplantation (FMT) – to restore microbial communities
- Prebiotics – to enhance beneficial microbial growth
- Probiotics – to introduce new microbial strains
- Synbiotics – combining pre- and probiotics
- Short-Chain Fatty Acids (SCFAs) – to deliver metabolic signals
Here’s what the data show:
➣ Prebiotics were linked to modest reductions in BMI and body weight, but no significant changes in waist circumference or body fat percentage.
➣ Synbiotics showed some effect on blood pressure in one trial, but inconsistent results for weight outcomes.
➣ SCFAs appeared to reduce BMI and waist circumference in early studies—though the research is still emerging.
➣ Probiotics showed minimal or no effect across multiple trials.
➣ FMT offered no clear benefit for BMI or waist circumference in adolescents.
Importantly, adverse events were rare and mild, mostly gastrointestinal symptoms.
Interpreting the Results: Why Were Effects So Limited?
From a clinical standpoint, one question naturally follows: If the microbiome is so central to metabolism, why didn’t these interventions produce stronger effects?
In my view, the answer lies in scope and context. Short-term, isolated microbiome interventions are unlikely to significantly impact pediatric obesity if broader dietary and lifestyle factors remain unchanged.
Obesity is not just about biology—it’s about systems. Without addressing the child’s full nutritional environment, movement patterns, sleep quality, and stress load, any single intervention is working upstream against entrenched patterns.
Clinical Takeaways for Integrative Pediatric Practice
While the data doesn’t support microbiome-based therapies as standalone solutions, it does support their thoughtful use as adjuncts within a whole-child approach.
Here are some evidence-informed ways to apply these findings:
🔹Start early: Childhood and adolescence represent a critical window for microbiome plasticity and metabolic reprogramming.
🔹Leverage dietary prebiotics: Foods like green bananas, onions, leeks, and Jerusalem artichokes feed beneficial microbes and are easy to include in child-friendly meals.
🔹Support SCFA production: Encourage intake of resistant starches and legumes to fuel butyrate-producing bacteria.
🔹Frame interventions in context: Gut-directed therapies should be paired with anti-inflammatory nutrition, adequate sleep, movement, and psychosocial support for meaningful change.
The Bottom Line
Microbiome-based interventions show potential, but current evidence suggests their effects on pediatric obesity are limited without broader lifestyle and dietary shifts. In my opinion, short-term interventions that do not address whole diet or lifestyle factors are unlikely to meaningfully influence obesity outcomes in children. This perspective is not a dismissal of microbiome science—it’s a call to integrate it more effectively within comprehensive care.
As research evolves, we can continue refining how we use gut-focused strategies in practice. But for now, the best results will come from viewing the microbiome not as a silver bullet—but as one important lever in a multifactorial model of care.
Want pediatric-focused insights that cut through the noise? Subscribe to my Monday Study Rundown, where I unpack new research and what it means for real-world care.
For more Monday Study Rundowns, click here.